
WHY VACCINE EQUITY MATTERS
“It shouldn't be an accident of birth”: How we ensure equal access to vital vaccines now and into the future.
COVID-19 has seen an unprecedented effort in medical research and discovery, but is access to vital life-saving interventions equal around the world? The vaccine alliance, GAVI, and COVID-19 Vaccines Global Access (COVAX) facility are focused on ensuring equitable access.
Burnet's vision is Equity Through Better Health, and there's no better example of where this is needed now than with the COVID-19 vaccines rollout globally.
“Everybody everywhere should have access to life-saving treatment, including vaccines. It shouldn't be an accident of birth as to whether you have access.”
And that commitment is also at the heart of the mission of GAVI, The Vaccine Alliance.

GAVI was set up in 2000 when vaccination rates were dropping globally, while at the same time a number of very powerful new childhood vaccines were coming on board, including for pneumonia and diarrhoea, which were responsible for the deaths of approximately 35 per cent of children under five years, particularly in lower-income countries.
However, the new vaccines were expensive, and children in lower-income countries weren't getting them.
The big pharmaceutical companies didn’t see these countries as markets to target because lower-income countries were seen as unreliable payers and/or intermittent purchasers. Essentially, children were missing out on life-saving vaccines because of market failure.
A group of creative thinkers from very different backgrounds (including Sir Gus Nossal) decided that the key to solving this problem was to intervene and shape those markets. As a result, GAVI was established as a new global health public, private, partnership.
By aggregating the huge volume of demand from lower-income countries and with secure funding from donors including Australia, GAVI was able to negotiate longer-term deals at much lower prices, while still allowing the manufacturers to turn a profit.

GAVI addresses market failure by securing long-term vaccine deals for much lower prices.
GAVI addresses market failure by securing long-term vaccine deals for much lower prices.
GAVI is currently a co-leader – with the Coalition for Epidemic Preparedness Innovations (CEPI) and the World Health Organization (WHO) alongside delivery partner UNICEF – of the COVID-19 Vaccines Global Access (COVAX) facility. In its first phase it aims to secure more than two billion doses to meet the needs of lower-income countries by the end of 2021.
It has been able to do this because it is the only established global health platform that pulls together governments, private sector, research institutions and civil society, and has a tested model and proven track record over 20 years of getting vaccines out to lower-income countries at affordable prices.
You're reading IMPACT magazine | Subscribe today
Donors, eligible countries, communities, and pharmaceutical companies trust GAVI, and this will be critical to GAVI’s ability to respond to the unique challenges presented by the COVID-19 pandemic, including the unprecedented pace of vaccine development.

Namibia received 24,000 COVID-19 vaccines through the COVAX Facility in April 2021. Image source: GAVI
Namibia received 24,000 COVID-19 vaccines through the COVAX Facility in April 2021. Image source: GAVI
The Global Fund to Fight AIDS, Tuberculosis and Malaria is a similar, established global health platform. It is co-convenor with FIND, a global diagnostics alliance, and WHO, to take the leadership in ensuring there are rapid and appropriate investments in diagnostics and testing capacity, which are also key tools in the fight against COVID-19. As with the COVAX facility, there is a commitment to ensuring that these tools will be equitably available to all countries.
The Global Fund has been able to pivot to allow its grants to support countries in terms of personal protective equipment, training and diagnostic development to address COVID-19; to adapt their HIV/AIDS, tuberculosis (TB) and malaria programs to be responsive to demands created by the pandemic; and to strengthen critical health and community systems.
These are a few examples of exactly what's needed and what’s happening on a grander scale – unprecedented and encouraging cooperation and collaboration between countries, big international organisations and the private sector, particularly the pharmaceutical companies.
Enlightened self-interest
The Australian Government’s response to the COVAX facility has been extremely positive. As a starting point, COVAX has committed to 20 per cent of population coverage for vaccines in countries that can’t afford to buy the vaccines. However, in addition to providing financial support to the facility, the Australian Government has also committed to fund the purchase of additional vaccines to ensure all Pacific Island countries will have 100 per cent coverage and to supplement the vaccines available to some other countries in the Indo-Pacific region.
Please support our COVID-19 research | Donate today
Just as importantly, Australia will be supporting and funding technical assistance for countries to roll out the vaccines and collaborating closely with other donor countries, so that low-income countries with limited resources are not having to separately manage multiple donors as well as the pandemic.
The fact that Australia was able to respond so quickly to the growing emergency in Papua New Guinea (PNG) with an initial dispatch of 8,000 doses of our own vaccine supply is very positive.
#PNG received its first shipment of 132,000 doses of AstraZeneca vaccines from the #COVAX Facility this morning. These vaccines will be offered first to health workers followed by other frontline workers at high risk of COVID-19 infection. Thank you COVAX partners and donors! pic.twitter.com/Q1YDMedqQc
— Anna Maalsen (@AMaalsen) April 12, 2021
The question now is how we keep going, because we shouldn’t for one moment think that once the vaccine is in place, the problem is solved. Health systems of lower-income countries such as PNG have been stretched to breaking point.
“The flow-on effect is that a multitude of health conditions and diseases including measles, pertussis, HIV, tuberculosis and malaria haven't received the attention and treatment that's needed and are on the rise again, so there's a lot of work to be done to catch up.”
We need the cooperation that we've seen with COVAX to continue, because it's in everyone’s interest to ensure that lower-income countries have strong health and education systems. That’s how sustainable development, peace and security is achieved – not just for the countries directly impacted, but for the region, including Australia.
“It will be vital to ensure that when the pandemic is over, we don’t simply revert to ‘business as usual’.”
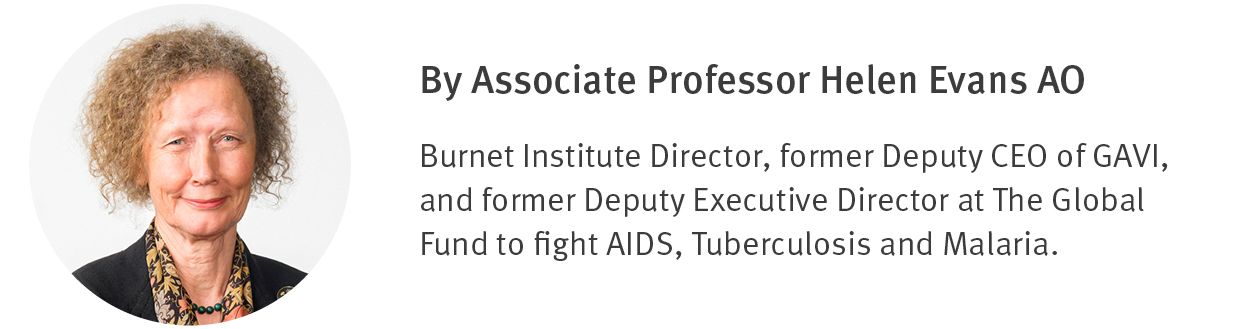
Associate Professor Helen Evans AO

Lessons from the pandemic
When the postscript to COVID-19 is written, one of the key chapters must surely focus on how the global response can be applied currently and in the future to other infectious diseases.
Peter Sands, the Executive Director of The Global Fund, noted we have better data on COVID-19 – where it is, where it’s heading, and how it’s changing – than we have on HIV, TB and malaria, even though we’ve been working on these other pandemics for decades.
So, we can do better on data. You can’t talk about leaving no-one behind, as the United Nations' Sustainable Development Goals do, if you don’t know who the people are, and if what you’re doing is effective.
Another lesson is that when the world gets behind it, vaccines can be produced incredibly quickly. Support for work on TB therapeutics and vaccines has been dragging the chain forever – it is the world’s deadliest infectious disease, and we’re still looking for a vaccine.
And there are lessons in what we haven’t done well with COVID-19. Too much top-down, undifferentiated communication is one, and it’s a reminder that we need to work closely with communities as key partners.
It’s my hope these lessons generate a swing away from inward-looking nationalism towards a recognition that we are all interconnected and need to work together.

Governing Health Futures Commission Co-Chair, Dr Anurag Agrawal
Governing Health Futures Commission Co-Chair, Dr Anurag Agrawal
At the UN General Assembly in September last year, Dr Anurag Agrawal, Co-Chair of the Governing Health Futures Commission said: “For the time being, fear has patched together all our differences, but I’m afraid that when this fear goes away, all these cracks that we’ve paved over temporarily will come back.”
I share his concern, so it will be vital to ensure that when the pandemic is over, we don’t simply revert to business as usual. When we get a chance to draw breath, we need to reassess and hopefully do better across the board.
It helps to be – as former Australian Senator and Age Discrimination Commissioner, Susan Ryan, once described herself – a persistent optimist. I think it would serve us all well to be persistent optimists.

Make an Impact | Donate Today
Please donate today and stand alongside Burnet Institute’s COVID-19 experts as they race to save lives. Your gift will give us the capacity and flexibility to respond where we see the greatest opportunity for impact.
Contact Us
If you would like to discuss this edition with our team please contact Tracy Parish.
E: communications@burnet.edu.au
T: +61 3 9282 2111
Where possible people who appear in images included in this publication were photographed with their permission. There is no implication that these people have any infectious diseases.
Stay across the latest from Burnet Institute
Subscribe to IMPACT magazine today
Discover the IMPACT of Burnet’s medical research breakthroughs and public health projects in the Institute’s bi-annual magazine.
