
LET EVERY VOICE BE HEARD
The Optimise Study gives Victoria’s non-English speaking communities the opportunity to contribute to policy.
While Afaf Mohamed was in and out of a Melbourne ICU with COVID-19 in mid-2020, she wasn’t aware that her family had also contracted the virus.
“I was in hospital for 37 days so I didn’t know what was happening outside, but when I came back my family had all been infected,” Ms Mohamed said.
Ms Mohamed contracted the virus from a family member, who was working at a hospital in the city’s inner suburbs. Fortunately, no-one else in her family was admitted to hospital, but lockdowns made it difficult for the close-knit South Sudanese community to rally around them in the way they normally would.
At the start of the pandemic, many culturally and linguistically diverse (CALD) communities in Melbourne struggled to access reliable and clear information about the virus in their language.
“Last year people didn’t have any information about COVID-19, but this year is not bad,” Ms Mohamed said.
“The pandemic has underlined the complexity of developing and implementing public health messaging for diverse communities during a crisis.”
Issues go beyond tailoring and translating information on getting tested, quarantining or getting vaccinated.
Since mid-2020, the Burnet and Doherty Institutes-led Optimise Study has gathered valuable insights from subsets of Victoria’s community who are at greater risk of COVID-19 and its effects, to inform government policies and strategies.
This has included CALD communities, who face language barriers, discrimination and difficulties accessing support services. Language and cultural barriers also make it difficult for researchers, but Optimise Study Coordinator Dr Stephanie Fletcher-Lartey says her team is overcoming this by employing five bilingual data collectors.
“By allowing someone from the community to lead the recruitment and capture that data, they can understand the nuances in the language,” she said.
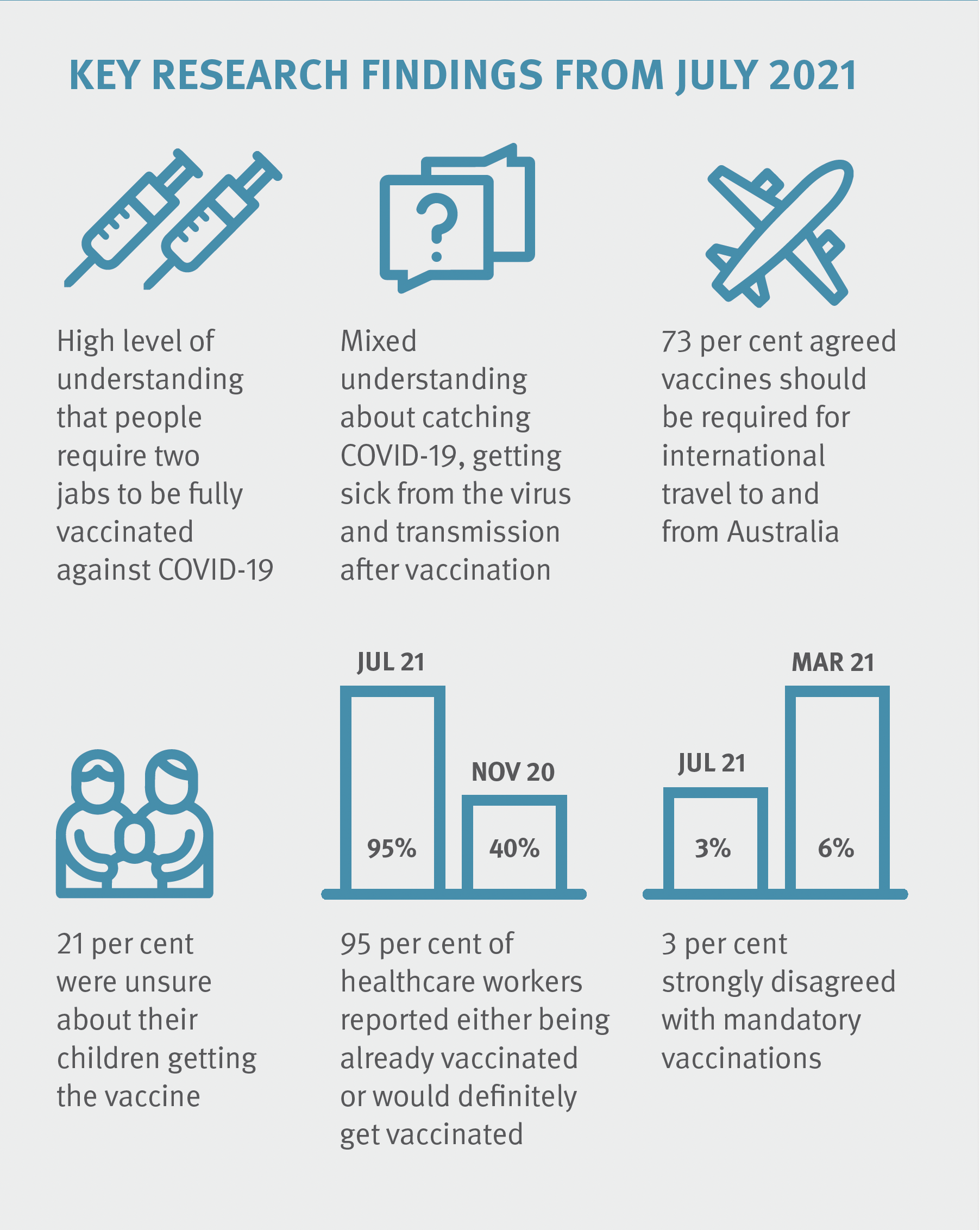
>> In July 2021, The Optimise Study led by Burnet and Doherty Institutes found that more than 86 per cent of Victorians in the study were ‘definitely’ intending to be vaccinated or already vaccinated for COVID-19, with significant increases reported among healthcare workers and people aged 35–44 years. This compares to November 2020 when 61 per cent of participants indicated their intention to be vaccinated.
You're reading IMPACT magazine | Subscribe today
Dr Fletcher-Lartey, a public health epidemiologist, said she and colleagues worked with Victoria’s Department of Health and the Centre for Culture, Ethnicity and Health to identify three priority languages: Arabic, Mandarin and Dinka.
“Arabic is the fifth most common language spoken in Victoria and is spoken by people from quite a diverse group of countries,” she said.
Mandarin is widely spoken in Victoria, but the Optimise team is also assessing the continuing impact of negative social media perceptions of Chinese communities due to the first cases of the COVID-19 virus emerging in Wuhan, China.
“The Dinka-speaking community is nowhere near as big. However South Sudanese in Victoria actually form part of very extensive family networks,” Dr Fletcher-Lartey said. “It can be difficult to limit social engagement, because that’s a very important part of their cultural setting.”
Dr Fletcher-Lartey says she is proud to work with the bilingual data collection staff.
“This now gives us the opportunity to genuinely say that we have captured information on a diverse group of participants from across Victoria,” she said.
Deng Malith, a member of Melbourne’s South Sudanese community, is one of the Optimise data collectors. His role is to recruit Dinka-speaking people into the study, and gather information from them and their networks. Mr Malith says having researchers from the community underlines to members of the community that they are being heard.
“It helps people understand that they have to take a role in it, their participation is important,” he said. “The way it has been designed is really helpful. The research will bring up information and data we have not seen.”
Part of this involves asking the right questions, and in the right way.
“When we trained our bilingual staff, one identified an issue in a response option in our survey: ‘prefer not to say',” Dr Fletcher-Lartey said.“This doesn’t make sense in Arabic, it actually implies something offensive. We reworded it to ‘I would not like to answer’ which is more respectful. We would not have otherwise picked up on that very small nuance.”
CALD study participants have already reported more severe impacts on their employment and mental health, and having smaller networks to rely on when isolating.
“Some of those things are crucial for us to pay attention to,” Dr Fletcher-Lartey said. “When we feed this back into our report to the [Victorian] government they will not just hear the voice of the ‘mainstream’, they’ll hear the voice of our broader diverse community.”

The Optimise Study is a partnership between Burnet Institute and the Peter Doherty Institute for Infection and Immunity, in collaboration with other organisations.
Find out more about The Optimise Study.
Please support our COVID-19 research | Donate today

Make an Impact | Donate Today
Please donate today. Your donation will enable us to focus on safe birthing in the time of COVID-19 to improve health outcomes for mothers and babies in Papua New Guinea.
Contact Us
If you would like to discuss this edition with our team please contact Tracy Parish.
E: communications@burnet.edu.au
T: +61 3 9282 2111
Where possible people who appear in images included in this publication were photographed with their permission. There is no implication that these people have any infectious diseases.
Stay across the latest from Burnet Institute
Subscribe to IMPACT magazine today
Discover the IMPACT of Burnet’s medical research breakthroughs and public health projects in the Institute’s bi-annual magazine.
