Virus decoy and 'immune harnessing' trialled for COVID-19
Burnet adds antibody expertise to hunt for drugs against coronavirus
Understanding how immune cells rally against a threat – and settle down again – is crucial in developing treatments that fight disease but don’t cause damage themselves.
It’s an area of expertise that Burnet researchers are bringing to a multi-organisational search for medicines for COVID-19, supported by almost AUD$2m from the Australian Government’s Medical Research Future Fund.
Head of Burnet’s Immune Therapies Group, Professor Mark Hogarth is leading the development of a series of unique biological drugs (which mimic naturally occurring proteins) in the consortium, of which three will enter preclinical trials by the end of 2020.
“Our commitment to understanding how antibodies stimulate the immune system through receptors called Fc receptors has been a three-decade effort, during which we pioneered much understanding of the ‘immune harnessing’ work of antibodies,” Professor Hogarth said.
He and colleagues from The University of Melbourne discovered several Fc receptors in humans in the 1980s and have worked on them ever since – research with broad applications including cancer, autoimmune diseases, and infections.
“Everybody’s got a particular expertise and class of biological drug they are bringing to the COVID-19 testing table. We will also provide input into the selection process, so the biologicals that will be trialled are the best virus-neutralising entities, and the best immune function stimulating entities.”
Professor Hogarth’s lab has engineered two human proteins into the one molecule in a bid to both prevent and treat COVID-19.
One end of their ACE2-Fc drug is a clone of the human ACE2 receptor – the ‘entry point’ that the SARS-CoV-2 virus uses to get into our cells.
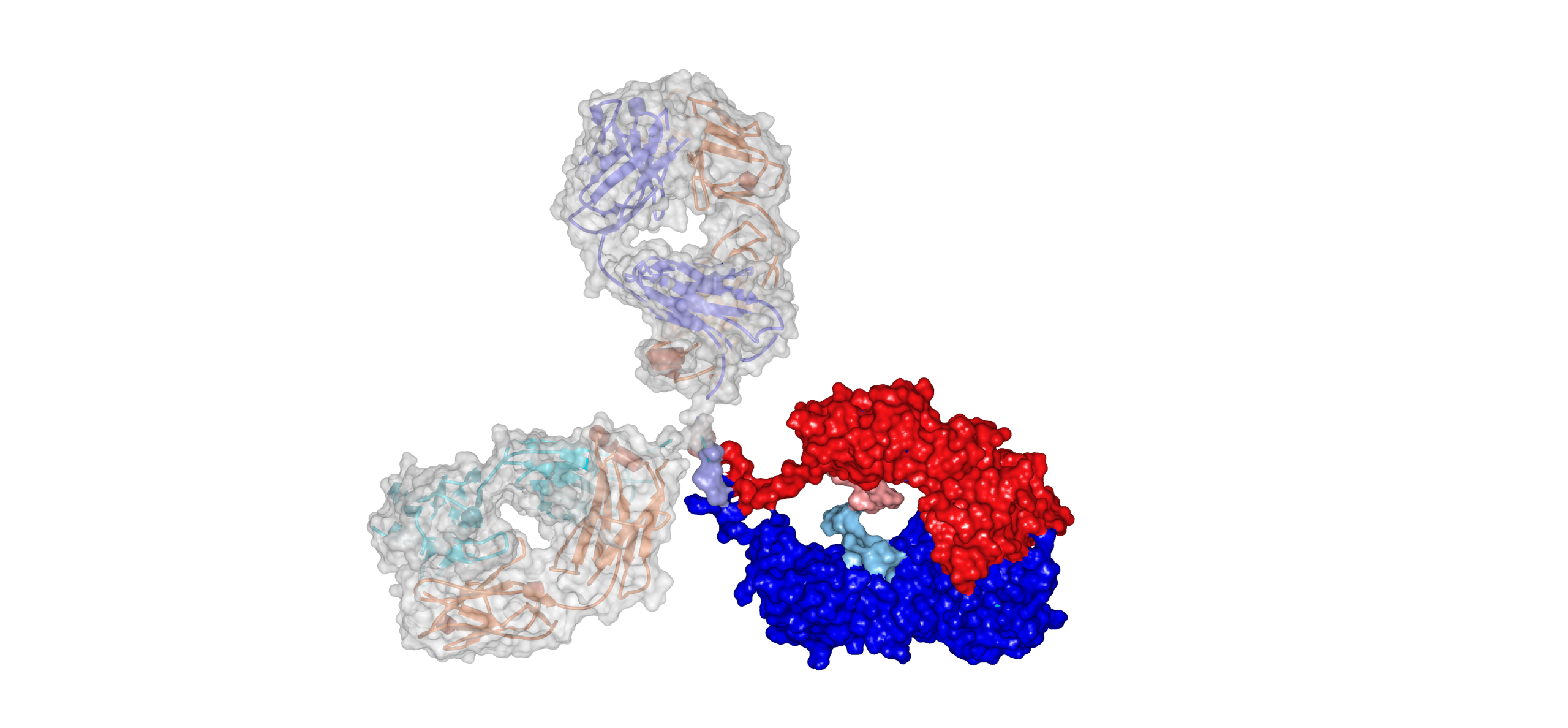
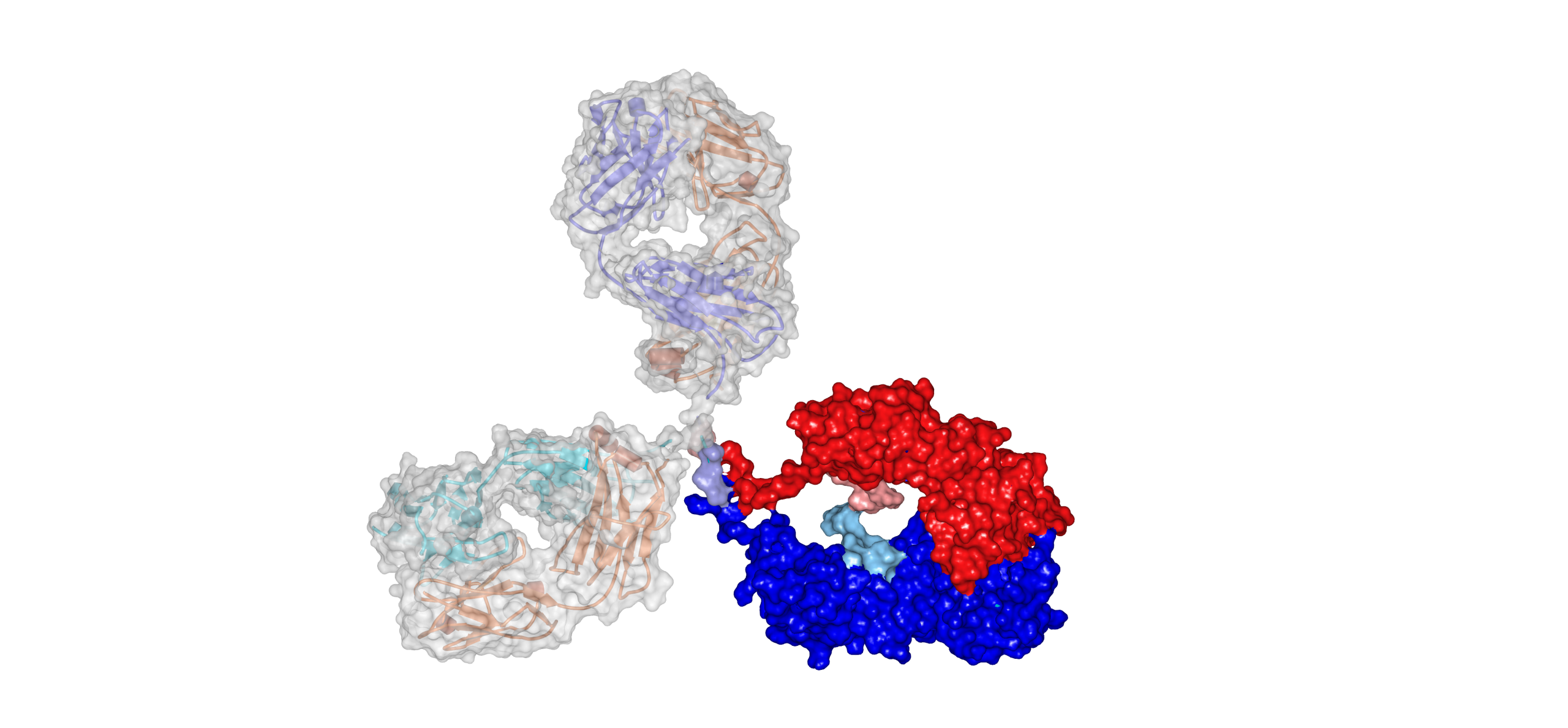
The x-ray crystal structure of an antibody. The immune stimulating Fc portion is composed of two chains shown in red and or blue. The virus neutralising Fab portions are uncoloured.
The x-ray crystal structure of an antibody. The immune stimulating Fc portion is composed of two chains shown in red and or blue. The virus neutralising Fab portions are uncoloured.
This clone acts like a decoy, stopping the virus entering and replicating within host cells, and has performed successfully in in vitro studies, Professor Hogarth said.
"This decoy will also be effective against any other coronavirus that uses ACE2 as its receptor, including the virus that causes SARS and any future coronaviruses," he said.

Professor Mark Hogarth in Burnet's Immune Therapies Laboratory
Professor Mark Hogarth in Burnet's Immune Therapies Laboratory
An important aspect of the drug’s Fc component is its ability to dial down an over-stimulated immune response, which caused worse disease in several animal trials for a SARS vaccine.
“We have a unique set of modifications that controls the immune-stimulating potential of the ACE-2 Fc and of antibodies,” he said.
“We’re one of few groups in the global research community that’s worked for so long on how antibodies and their Fc receptors really control the immune system. We are applying this experience from our cancer and inflammation studies to the prevention and cure of COVID-19.”
Please donate to support our COVID-19 response.
