Burnet’s role in
COVID-19 vaccine quest
"It's all consuming"
Researchers are manipulating the ‘key’ SARS-CoV-2 uses to break into our cells
Professor Heidi Drummer has always been fascinated by viruses – which is lucky, because now she spends up to 10 hours per day thinking about one virus in particular.
“I wake up thinking about SARS-CoV-2. The work on a vaccine has been really consuming,” Professor Drummer, Burnet’s most senior virologist, said.
While hundreds of research groups around the world are working frantically to create a vaccine against COVID-19, the disease caused by the SARS-CoV-2 virus, a team at Burnet is taking a unique approach guided by decades of research on other viruses.
“Several vaccines around the world have now entered human clinical trials, and all of them include the surface spike protein of the SARS-CoV-2 virus, which is the primary target of neutralising antibodies in our immune system,” Professor Drummer said.
The spike protein is particularly important because it acts like a key to unlock the ‘photocopy room’: it gets the virus into our cells, where it can hijack the machinery and copy itself over and over.
Professor Drummer said the other groups are using the spike protein in its natural form.
But Burnet’s COVID-19 Vaccine Development team of five researchers, led by Dr Andy Poumbourios and Professor Drummer, is tweaking the spike protein so it attracts more focused attention from the immune system, without sending the response into overdrive.
“Our approach is to change the structure of the spike protein into one that will generate an antibody response that will be protective, but have no ability to cause what’s called antibody-dependent enhancement (ADE), where the disease is worse in vaccinated people.”
Professor Heidi Drummer

ADE halted the development of several vaccines against SARS (now SARS-CoV-1), when reports emerged that animals suffered worse disease when exposed to the virus if they had been vaccinated.
The Burnet team plans to put several of its best-performing spike proteins into animal trials in October 2020, with early results expected before year’s end.
The work is a natural transition for Professor Drummer; for almost 20 years she has been studying what makes certain viruses so good at evading our immune systems.
“A major focus for my career has been understanding how viruses attach to receptors on our cells and then how they rearrange their structure to get into the cell,” she said.
“The flip side is, how does the immune system see the virus? And how can we make better antigens – which stimulate an immune response – for vaccines?”

Lessons from other viruses
During her PhD, awarded in 1993, Professor Drummer helped to identify new parts of the influenza virus that T cells (a type of white blood cell) bind to when they attack.
She later studied the role of various adjuvants (substances added to vaccines to boost the immune response) for the influenza vaccine, and the proteins on the surfaces of human immunodeficiency virus (HIV) and human T cell lymphotropic virus (HTLV).
Professor Drummer and Dr Poumbourios have been working for years on a vaccine to protect against all eight of the circulating genotypes of hepatitis C virus (HCV), securing three patents on their technology. This has included re-engineering the protein that helps the virus enter our cells.
“If you just immunise people with the ‘native’ HCV glycoprotein, it’s incredibly hard to get a protective immune response because HCV has immune-evasion mechanisms that minimise the amount of neutralising antibodies our bodies make, and restrict the ability of those antibodies to recognise other strains of virus,” Professor Drummer said.
“This has been a really intractable problem for HCV vaccine research. A lot of my work has been on trying to re-engineer those HCV surface proteins so they better stimulate these broadly reactive neutralising antibodies, which are effective against lots of different strains of HCV. Hopefully then we can use one antigen to protect against many different strains of the virus.
“When COVID-19 happened, we saw an opportunity to transfer what we’ve learned from HIV, HTLV, and HCV, to see if we can generate really strong, long lasting neutralising antibodies.”
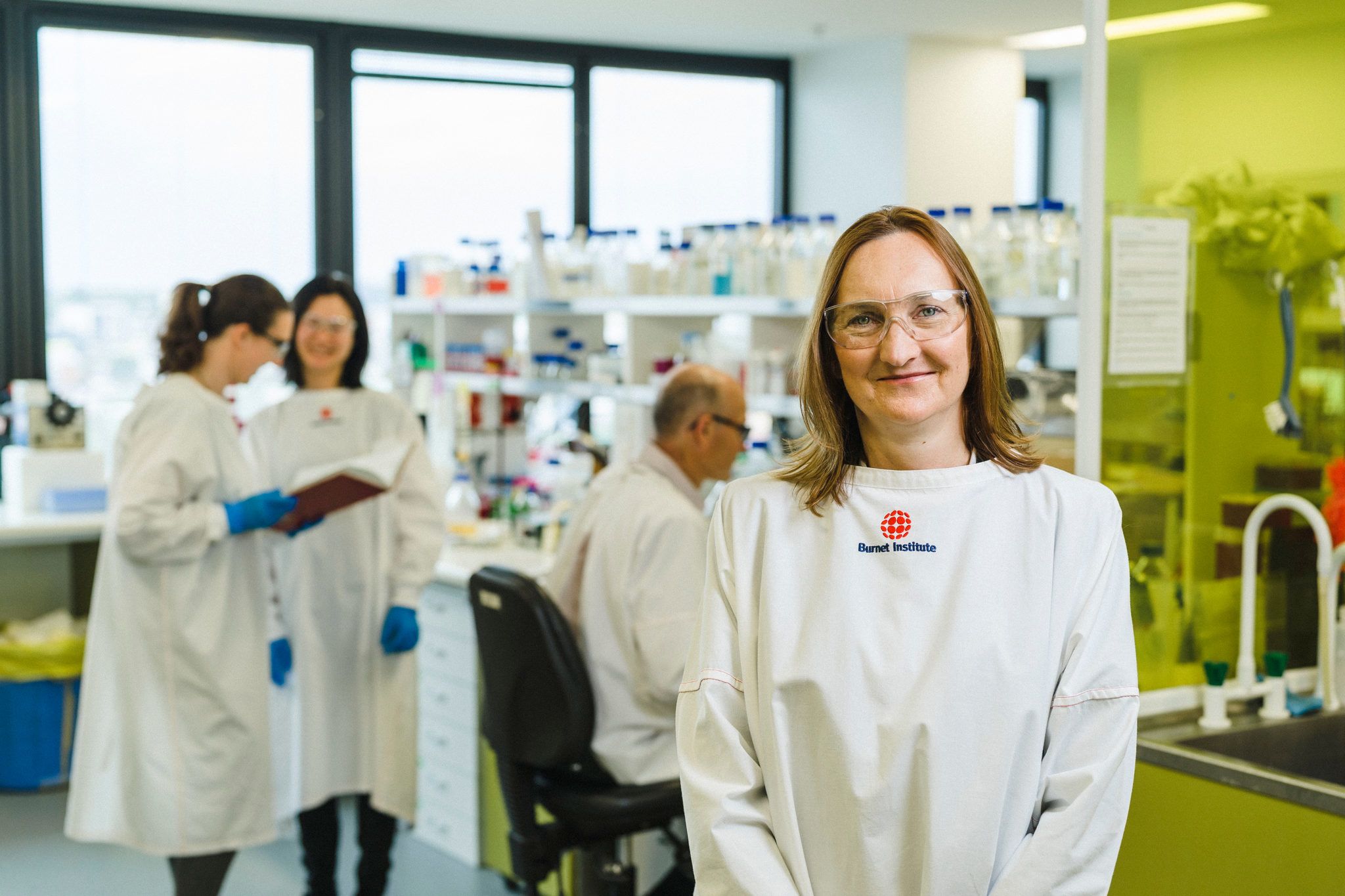
Felicia Schlotthauer, Irene Boo, Dr Rob Center and Professor Heidi Drummer in Burnet's Viral Entries and Vaccines Laboratory
Felicia Schlotthauer, Irene Boo, Dr Rob Center and Professor Heidi Drummer in Burnet's Viral Entries and Vaccines Laboratory
Despite the intense focus, securing a vaccine will be a long process, she said.
“There has been an incredible, unparalleled global response to this pandemic, even going beyond what we did for HIV, but I think we’re still a couple of years away from a vaccine.
“What happens in the next 18 to 24 months in vaccine development will be really interesting: they’re going to require big phase III studies, to prove that ADE doesn’t happen, and to manufacture and distribute it.”
As to whether Australia will have the necessary manufacturing capacity will depend on the type of vaccine that performs best in clinical trials, Professor Drummer said.
“Then we’ll need to find a way of immunising everyone. Even with vaccines currently available, it’s hard to vaccinate people – you can’t just say ‘come and get it’, because people don’t behave that way.”
And while each team wants to be first, others’ successes will not mean the work stops.
“Several international research groups have published early results of COVID-19 vaccines tested in humans and the results look promising, with all generating an immune response and most having excellent safety profiles,” Professor Drummer said.
“But large, multi-country trials will be needed to fully examine their safety in diverse populations and ability to protect from infection and disease. As such, it’s essential that as many vaccine candidates are progressed as possible, so we have multiple options to augment the international vaccine effort and provide new knowledge about SARS-CoV-2 vaccine design and immunity.”
In the meantime, their team is happy to be contributing, Professor Drummer said.
“As a virologist, you almost have a duty to help in some way. Everybody in the lab is inspired to work on it – we feel we’ve got to do something, to lend our expertise to find a solution for this.”
How difficult is it to attract funding?
“Some organisations were already working in epidemic preparedness, whereas for groups like us who’ve come from a different field and perhaps come into it from a different angle, it’s been much harder to get funding,” Professor Drummer said.
“We’re basically running on limited funds and applying for every grant opportunity to progress this work."
Watch Professor Heidi Drummer explain Burnet's contribution to the global COVID-19 vaccine effort.
Please donate to support our COVID-19 response.
